
An Introduction and Guide to Dental Sleep Medicine.
Nearly everyone has experienced nights when they don’t get good sleep or don’t sleep much, and they wake up feeling “fuzzy” the next day. When we sleep, we go through several sleep cycles, including light sleep, deep sleep, and REM sleep (dreaming). Ideally, a sleep cycle takes about 90 minutes. Adults should have four to five 90-minute cycles of sleep each night.
However, if someone wakes up mid-cycle, the cycle starts over. A person with a sleep breathing disorder might restart the sleep cycle more than 18 times per hour, which reduces how much deep sleep (which is restful sleep) and REM sleep (which is active sleep) that person gets.
Deep sleep and REM sleep are extremely important, and scientists are learning more and more about what happens to the brain during sleep. A 2013 study funded by the National Institutes of Health (NIH) suggests that sleep is important in “cleaning” the brain.

Maiken Nedergaard, M.D., D.M.Sc., co-director of the Center for Translational Neuromedicine at the University of Rochester Medical Center in New York, led a study about what happens to the brain during sleep. For the study, researchers injected dye into the brain cells of mice while monitoring their electrical brain activity. The researchers observed the brain cells while the mice were in deep sleep. According to an NIH press release, the “space inside the [mice] brains increased by 60 percent when the mice were asleep or anesthetized.” This space allowed cerebral spinal fluid and blood to flow through the brain and remove the plaque that had built up on the brain throughout the day.
The study suggests that sleep clears the brain of “damaging molecules associated with neurodegeneration.” Although this was not a human trial, the theory suggested by the study is that the less deep sleep one gets, the less time the brain has to be cleaned. Thus, the research appears to support all the adages about “getting a good night’s sleep” or “sleeping on it” when approaching an important decision. The NIH press release said, “A good night’s rest may literally clear the mind.”
BACKGROUND
With it becoming increasingly clear that sleep is critical to overall health, all dental professionals should be educated about the risks of sleep breathing disorders and know the benefits of treatment. Dental professionals and medical doctors are on the frontline for patients who have questions and concerns about sleep problems.
Medical doctors and dental teams typically work together to help their patients with sleep breathing disorders. Patients often ask questions about whether insurance will cover sleep treatments, and how much it will cost. Dental professionals should be able to educate patients on the benefits of reducing the number of sleep disruptions through oral appliance therapy, if appropriate, or possibly opening up the nasal passage so that patients don’t have as many arousals an hour.
I began my career as a dental assistant in a “Barnesified” practice in Colorado. When I joined the team, our practice had already attended several Dr. Dick Barnes Group seminars, and we were implementing many principles of their philosophy. Because of this, our team dove into dentistry a bit deeper than most general dental practices.
We became involved in full mouth reconstruction cases and rebuilding patients’ occlusion and function. We also became interested in what dental practices could do to evaluate and improve patients’ airways.
In 2008, I took a job with software company called Dental Writer. While working for them, I attended several dental sleep medicine (DSM) courses around the country, listened to a number of speakers, and learned how they integrated DSM into their practices. With my background as a dental assistant, I was naturally interested in figuring out how to make this happen.
SLEEP BREATHING DISORDERS
Sleep breathing disorders happen when an airway collapses during sleep. Chronic, loud snoring is a common symptom. To be diagnosed with obstructive sleep apnea (OSA) as an adult, patients must meet the following criteria: stop breathing for 10 seconds or longer during sleep, have the oxygen saturation in their blood drop anywhere from 3 to 4 percent, and have it all happen five times or more an hour.
Another sleep disorder that can affect breathing at night is upper airway resistance syndrome (UARS). UARS is a common sleep disorder that is most often characterized by the narrowing of the upper airway, which causes sleep disruptions called respiratory effort-related arousals (RERAs). These arousals are a constant irritant that can be very taxing on the body.
According to the American Sleep Apnea Association (ASAA), OSA affects an estimated 22 million Americans. Sadly, 80 percent of moderate to severe cases of OSA have not been diagnosed. And it’s not just the patient’s physical health that is suffering—it’s costing billions of dollars and taking a toll on emotional health because of crabby days and irritable living.
Last year, the American Academy of Sleep Medicine™ (AASM) released an analysis called “Hidden health crisis costing America billions.” The analysis summarized the financial implications of undiagnosed OSA. On its website, the AASM notes that the consulting firm of Frost & Sullivan estimates that an “annual economic burden of undiagnosed sleep apnea among U.S. adults is approximately $149.6 billion. The estimated costs include [among other costs] $86.9 billion in lost productivity, $26.2 billion in motor vehicle accidents, and $6.5 billion in workplace accidents.”
Research shows that sleep disorders may also be linked to a variety of other diseases, including high blood pressure, diabetes, and even some types of cancer. Once I learned about the many implications of undiagnosed sleep disorders, I urged all my family members to get tested. Sure enough, we learned that nearly everyone in my family has a sleep breathing issue. I even learned that I have UARS.
Since sleep disorders affected so many family members, I started thinking about how many patients might benefit if more dentists integrated DSM into their practices. As dental professionals, it’s our job to ask patients whether they have had their sleep evaluated if we see any of the following health problems: high blood pressure, a history of heart attack or stroke, diabetes, cancer, acid reflux, depression, or daytime sleepiness.
In addition, we should be vigilant in looking for dental signs that could be linked to OSA like worn teeth from clenching and bruxing, a retruded mandible, a scalloped tongue, a high palatal vault, or a red soft palate.
MEDICAL TREATMENTS
Dental professionals should always keep in mind that sleep-disordered breathing is a medical condition. A dentist cannot diagnose it and proceed with treatment without working with a physician. Fortunately, there are several treatment methods, depending on the severity of the diagnosis and patient preference.
For UARS, treatment usually focuses on opening up the nasal passages. Sometimes that means that an ear, nose, and throat (ENT) doctor will have to perform surgery to open up that passageway.
For less severe diagnoses, non-surgical methods may be sufficient. Nasal strips can be an option, or nose cones that go up the nose to keep the nasal airway open may be helpful. Oral appliance therapy (OAT) may be another great option.
For OSA, most physicians prescribe a continuous positive airway pressure (CPAP) machine. This machine supplies constant air pressure through a mask or nosepiece that patients wear while sleeping. However, patient compliance is an issue with CPAP therapy. Many patients either remove the mask in the middle of the night or do not use it at all because it is uncomfortable, or they can’t tolerate having a machine blowing air into their airway all night.
A dental oral appliance may be used in conjunction with CPAP therapy through combination treatment or as an alternative to CPAP therapy if a patient is unable to wear or tolerate the CPAP machine.
For severe cases, physicians may recommend surgery to remove soft tissues in the back of the throat to keep the airway open. But some statistics show that this surgery may only last about a year before relapse. A local ENT doctor once told me that his surgeries are typically about 40 percent successful.
Another option may be a surgery called a maxillary mandibular advancement surgery, which involves pulling the upper and lower jaw forward, which works well to open up the airway. This surgery has a high success rate, but it is a major surgery.
THE ROLE OF DENTISTRY
Maintaining an open airway during sleep is essential. Therefore, in my opinion, oral appliance therapy may be necessary. Dentists can help patients keep their airway open with OAT or with other treatments, like expansion of the maxillary or mandibular jaw (this is performed mostly in pediatrics, but I’ve witnessed many adult cases, too), or possibly comprehensive dentistry.
Oral appliances are popular in dentistry right now. They are considered durable medical equipment, so they need to go through U.S. Food and Drug Administration (FDA) clearance to ensure that they can open and maintain a person’s airway.
Making oral appliances for sleep-disordered breathing is not new. The first oral appliances were made in the 1970s. In 1995, the AASM published its first ever parameters regarding OAT. Still, OAT didn’t become a hot topic until as recently as 2011—when Medicare announced that custom-made oral appliances for OSA would be a covered benefit.
Medicare’s policy is that only a dentist can offer oral appliances, and in many cases Medicare sets the standard that many private insurance companies follow. However, not all private insurance companies follow the same guidelines. I advise dentists to use a manufacturer that is making FDA-cleared oral devices, which means that they’ve undergone a vetting process by the FDA with regards to the manufacturer and lab. To use benefits from medical insurance for your patients, you have to follow their rules.
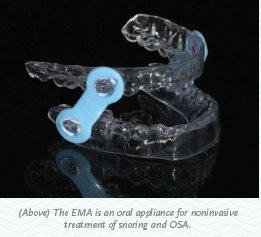
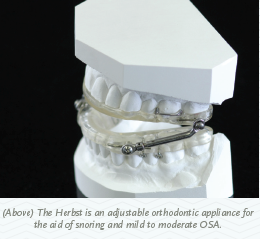
Arrowhead Dental Laboratory offers two oral appliances, the EMA appliance and the Herbst appliance. There are many more appliances available that are also FDA-cleared.
COMPREHENSIVE DENTISTRY
To find patients who are undiagnosed with dental sleep issues, consider including the following questions on the dental medical history questionnaire: “Have you ever had a sleep test? Has anyone ever told you that you have obstructive sleep apnea? Do you snore?”
If you conduct a brief new patient interview in conjunction with a health history questionnaire, it’s easy to start talking to patients and educating them about sleep issues. Dental team members can follow up with patients by asking, “Did you know that snoring can indicate an obstruction in your airway? We know now that when you have an obstruction, it can impact your overall health and wellness. We should have you evaluated and see what we can do.”
If patients are not yet diagnosed with a sleep breathing disorder, the dental team can arrange an appointment with a physician to get an evaluation. If the patient is already diagnosed, establish a protocol with your dental team to learn what therapies he or she is using, and offer additional support. Evaluating a patient’s airway should be part of a comprehensive dental exam.
GETTING STARTED
Any practice looking at implementing dental sleep medicine should consider taking an airway course that will allow dental teams to evaluate the patient prior to diagnosis. Once some initial education is obtained,dentists can decide if they want to implement DSM treatments slowly or more aggressively.
Some practices may just want to do an appliance or two a month and help their existing patients. But other dentists realize there is a bigger potential and may decide to stop doing general dentistry altogether to specialize in DSM. For the last two and a half years, I have worked with offices to help them analyze what to implement in terms of DSM, and strategize about how to make it happen. Typically, an exclusive DSM practice usually has relationships with physicians in the community who refer patients to the dentist for oral appliance therapy.
A specialty DSM practice might not do any general dentistry at all, but they likely offer ancillary treatments like position therapy—this focuses on different sleeping positions patients can use to keep them off their backs (typically airways collapse most often when patients sleep on their backs).
Practices that opt for the exclusive route typically have to develop relationships with physicians and get referrals coming in quickly. Once they are well known in the community, the practice can start to see results.
BILLING
With general dentistry, dentists and their teams have learned to overcome the “insurance barrier.” Even though insurance only pays a certain amount for some procedures, and may not offer benefit for others at all, it hasn’t stopped dental teams from educating patients about what they need so that they can make the decision to move forward.
Dental sleep medicine is similar. Dental practices have the power to help patients keep their airways open while they sleep. It’s about informing the patient, so the patient can make an educated decision to act.
Only patients who are diagnosed with OSA can use traditional medical insurance for reimbursement. With something like UARS, patients are usually unable to draw upon medical insurance benefits.
Insurance benefits depend on the severity of a patient’s condition. If the patient has mild OSA, a doctor typically needs to prove that the patient truly needs treatment. Most insurance companies will require one of seven medical conditions to be present in the patient in order to qualify for the benefit.
If a patient has severe OSA, which means that they stop breathing 30 times or more an hour, most insurance policies consider the therapy medically necessary when the patient is CPAP or PAP intolerant or contraindicated.
EDUCATION AND CERTIFICATION
There are several ways to get education and certifications for DSM. One organization that I recommend is the American Academy of Dental Sleep Medicine (AADSM). The AADSM is very research-based. They have educated dentists who have been helping patients and making oral appliances for about 26 years. If a dental office is interested in getting involved in DSM, they can go through the AADSM to apply for facility accreditation.
Dentists can work towards “diplomate” status, which means that dentists have to take an exam and submit cases to qualify. I consider diplomate status through the AADSM to be the “gold standard.” Because DSM education has blossomed in popularity recently, the academy sets standards to ensure that dentists are getting qualified education.
Alternatively, in the past five years, several other academies and teaching institutes have started their own certifications. Another great institution is the American Thoracic Society (ATS). It is a medical group, but they include dentists in a lot of their education.
The AADSM recently released a “qualified dentist designation” that provides a way for dentists to receive qualified education through a university-based setting, or through a not-for- profit organization. They require 25 continuing education credits to earn the designation. Courses are available at places like the Pankey Institute (where I am on faculty), through a university, or through the AADSM.
I also co-teach a course for the Dr. Dick Barnes Group seminars called Airway Management and Dentistry, which is a good introduction to DSM. It’s a great way to learn if you are interested in gaining certification through the accredited agencies.
Once you become knowledgeable about dental sleep medicine, turn to your inner circle to look for cases. Reach out to your family, dental team, and friends to discover who you can help and to gain valuable practice while learning the intricacies of dental sleep medicine. It’s a great way to become comfortable with the specialty. From there, the sky’s the limit!









