Dentists have been increasingly requesting zirconia as an alternative to porcelain-fused-to-metal (PFM) restorations, and more recently to glass ceramic restorations as well. In particular, for more than 15 years, zirconia has been used for fabricating restoration frameworks because of the material’s versatility in mechanical and physical properties, which has allowed clinicians and laboratory technicians to use it for various clinical indications.
Differentiated by a number of factors—including composition, mechanical characteristics, and optical properties—today’s new zirconia materials enable dentists and laboratories to choose among options that can be milled to full contour, demonstrate acceptable aesthetics, and offer translucency suitable for clinical situations that are ideal when high mechanical stability, thin restoration walls, and natural aesthetics are essential.
Questions about Zirconia
Many dentists have questions about dental zirconia materials, and confusion is common. Is it zirconium or zirconia? Is zirconia a metal? What do we use in dentistry? Dental zirconia (ZrO2) is the oxide version of zirconium (Zr). Zirconium occurs in nature only as a mineral, mostly as zircon (ZrSiO4), and is a soft, ductile, shiny-silvery metal, optically similar to aluminum foil.1,3 To produce dental zirconia, zircon is purified via complex production and purification processes, and then converted into synthetic zirconium precursors that are transformed into ZrO2 through thermal and mechanical processes. These are the only synthetic powder components that are used to make dental zirconia.1-3
Zirconia is polymorphic ceramic; meaning, depending on temperature and pressure, the same elements of the material exist in three different crystal structures, including monoclinic (m), tetragonal (t), and cubic (c). (See Figure 1.) Pure monoclinic zirconia, the most stable phase, is present at room temperature. However, this phase has the weakest mechanical properties, and hence can be milled fast and efficiently without damaging milling machines and tools.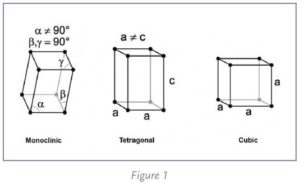
At about 1170° C, the monoclinic phase transforms into the tetragonal phase, with an approximately 4% to 5% volume shrinkage. At about 2370° C, the tetragonal phase then converts into the cubic phase. These transformations occur within a temperature range, not at a specific temperature, and involve movement of atoms within the crystal structure.
The tetragonal and cubic phases of zirconia can be made stable at room temperature by incorporating additional components (dopants) such as yttrium oxide (Y2O3), calcium oxide (CaO), or magnesium oxide (MgO) into the ZrO2 crystal structure to form partially or fully stabilized zirconia.1-3
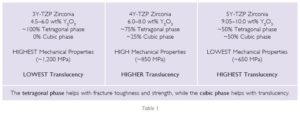
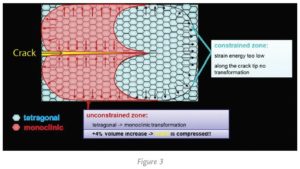
Without the addition of these dopants, tetragonal crystals convert back into monoclinic below 950° C, and hence cannot be used clinically. (See Figure 2.) Low amounts of these 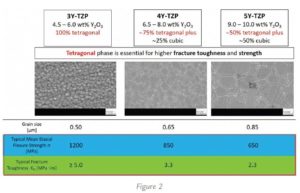 dopants lead to partially stabilized zirconia, with mainly metastable tetragonal and cubic phases.1-3 The quantity of dopant in molar concentration used in a zirconia is abbreviated as, for example, 3Y-TZP for 3 mol% Y2O3, 4Y-TZP as 4 mol% Y2O3, or 5Y-TZP as 5 mol% Y2O3. When approximately 4.5–6 wt% (3 mol% or 3Y-TZP) yttria is added to a structure, a 100% tetragonal phase (traditional dental zirconia) can be produced at room temperature.
dopants lead to partially stabilized zirconia, with mainly metastable tetragonal and cubic phases.1-3 The quantity of dopant in molar concentration used in a zirconia is abbreviated as, for example, 3Y-TZP for 3 mol% Y2O3, 4Y-TZP as 4 mol% Y2O3, or 5Y-TZP as 5 mol% Y2O3. When approximately 4.5–6 wt% (3 mol% or 3Y-TZP) yttria is added to a structure, a 100% tetragonal phase (traditional dental zirconia) can be produced at room temperature.
When approximately 9.0–10.0 wt% (5 mol% or 5Y TZP) yttria is added, a structure of 50% tetragonal/50% cubic phase (known as cubic or HT zirconia) can be produced at room temperature. When these powders are mixed, an approximately 6.5–8.0 wt% yttria containing zirconia can be produced (4 mol% or 4Y TZP), giving a microstructure of 75% tetragonal and 25% cubic. (See Table 1.)
The composition of zirconia material defines its mechanical and physical properties, and hence, clinical indications. The biaxial flexural strength of zirconia materials ranges from 650 MPa (5Y-TZP) to 1,200 MPa (3Y-TZP). The higher the value, the stronger the material. In addition, the presence of polymorphic phases in zirconia material provides a phenomenon called “phase transformation toughening.” It causes the tetragonal crystals to change to monoclinic when a crack is introduced. The monoclinic phase has a greater volume. This stops the crack from traveling through the material, basically pinching the crack shut (see Figure 3), and hence further increases resistance to fracture.
No phase transformation toughening can be observed in 5Y-TZP materials. Lastly, the translucency of 3Y-TZP is comparatively lower than 4Y-TZP and 5Y-TZP (most translucent), resulting in a clinical decision-making tree for clinical indications and cementation procedures.
The first zirconia restorative materials on the dental market were 3Y-TZP powders. Although these materials had high mechanical properties, they were dense and opaque, falling short of dentists’ requirements for aesthetics, which were as important as strength considerations. Since then, varieties of zirconia materials (such as 4Y-TZP and 5Y-TZP) have become available to meet dentists’ different functional and aesthetic demands.
Today’s Different Zirconia Materials
As discussed earlier, the obvious disadvantage of new higher translucency and more aesthetic ZrO2 materials is reduction in the mechanical properties (e.g., lower fracture toughness and/or lower flexural strength).4,5
Currently, newer generation cubic—5Y-TZP (e.g., CubeX2)—or hybrid—4Y-TZP (e.g., IPS e.max® ZirCAD® MT)— zirconia materials are limited to single-unit restorations to three-unit bridges. Such zirconias exhibit improved translucency for aesthetic full-contour (i.e., monolithic) restorations, but they demonstrate lower mechanical properties and a reduction in strength and fracture toughness compared to some other restorative materials.6,7 This may limit their use to certain indications, wall thicknesses, and connector dimensions.
The 3Y-TZP zirconia materials (e.g., IPS e.max® ZirCAD® LT) are indicated for single-unit restorations to multi-unit bridge frameworks with a maximum of two pontics. Such materials demonstrate high strength, excellent mechanical properties, and a low risk of temperature degradation; however, they exhibit a slightly lower level of translucency8.
The existence of a variety of zirconia materials creates confusion and excessive inventory for dental laboratories. In addition, clinicians should follow tooth preparation guidelines specific to their selected zirconia restorative material. It is critical for both clinicians and dental laboratory technicians to consider the differences in properties among zirconia materials when selecting the ideal zirconia for a specific clinical indication.
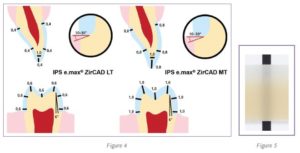
Preparation guidelines for 3Y-TPZ zirconia materials range from 1.0 mm to 0.5 mm occlusal and axial reduction, whereas for 4Y-TZP and 5Y-TZP zirconia restorative materials, they range from 1.5 mm to 1.0 mm reduction. (See Figure 4)Additionally, the connector dimensions for bridges vary from 12.0 mm2 for 5Y-TZP and 4Y-TZP materials to 7.0 mm to 9.0 mm2 for 3Y-TPZ zirconia materials.
IPS e.max® ZirCAD® Prime
 The newest generation of zirconia restorative material—IPS e.max® ZirCAD® Prime—is the next generation of all-ceramic restorations. This revolutionary material ensures exceptional quality of aesthetics and offers all indications ranging from single unit to long-span bridges with 14 units. Hence, it provides a complete solution for both dental technicians and clinicians. The unique “gradient technology” (GT) allows two zirconium oxide raw materials—3Y-TZP and 5Y-TZP—to be combined into one puck, allowing for the strength of 3Y-TZP and the aesthetics of 5Y-TZP. This technology involves three innovative processing steps:
The newest generation of zirconia restorative material—IPS e.max® ZirCAD® Prime—is the next generation of all-ceramic restorations. This revolutionary material ensures exceptional quality of aesthetics and offers all indications ranging from single unit to long-span bridges with 14 units. Hence, it provides a complete solution for both dental technicians and clinicians. The unique “gradient technology” (GT) allows two zirconium oxide raw materials—3Y-TZP and 5Y-TZP—to be combined into one puck, allowing for the strength of 3Y-TZP and the aesthetics of 5Y-TZP. This technology involves three innovative processing steps:
- Optimized conditioning of indigenous powders to adjust the sintering kinetics of 3Y-TZP and 5Y-TZP for uniform shrinkage.
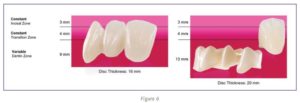
- Proprietary, state-of-the-art filling technology, which allows IPS e.max® ZirCAD® Prime to offer a true material progression from dentin to enamel. Unlike multi-layered materials on the market that can have visible layers of color and offer no change in material composition (as they are merely stacked layers of pigmentation), GT offers a seamless progression of shade and translucency to provide premium aesthetics combined with exceptional strength. (See Figure 5.)
- High-quality pressing technology, which is distinct from traditional ceramic material that utilizes one type of manufacturing process. IPS e.max® ZirCAD® Prime is created through multiple processing steps. One of these is cold isostatic pressing (CIP). In this step, the discs are uniformly compacted from all sides simultaneously. This improves the microstructure of the material and optimizes its translucent properties. Furthermore, it allows the material to be sintered at shorter intervals.
An intelligent disc concept allows a lab technician to position a restoration per clinical requirement and indication. The incisal and gradient zone of the IPS e.max® ZirCAD® Prime discs are always the same height, whereas dentin zone differs depending on disc thickness. (See Figure 6.) In addition, it offers all processing techniques—including staining, infiltration, cut-back, and layering—to achieve desirable results. Therefore, IPS e.max® ZirCAD® Prime is one material for all solutions.
Cementation Protocol
 IPS e.max® ZirCAD® Prime provides flexibility for clinicians to use all cementation options (e.g., conventional, self-adhesive, and adhesive cements). It is important to remember the actual cementation technique and diligently follow the protocol because it influences clinical success.
IPS e.max® ZirCAD® Prime provides flexibility for clinicians to use all cementation options (e.g., conventional, self-adhesive, and adhesive cements). It is important to remember the actual cementation technique and diligently follow the protocol because it influences clinical success.
Clinicians often use conventional cements (e.g., resin-modified glass ionomers, or glass ionomers) when placing zirconia restorations due to their ease of use. However, the limited bonding properties of conventional cements restrict their use in non-retentive tooth preparations.
The common myth is that zirconia material cannot be chemically bonded. However, highly-cited literature shows that zirconia restorations can be chemically bonded. The self-adhesive cements like SpeedCEM® Plus offer ease of use like conventional cements, and provide chemical bonding for long-term success.
To ensure successful cementation, use the following protocol. Avoiding any step in the cementation protocol will compromise the clinical outcome.
- Air-abrasion of the intaglio surface of restorations using Al2O3 particles (50 µm) at 1 bar pressure—which is usually performed by the dental laboratory—roughens the zirconia surface to increase micro-retention for improved bonding.
- After trying-in the restoration in the patient’s mouth, it should be cleaned. Zirconia surfaces show a high affinity for phosphate groups, and saliva and other body fluids contain various forms of phosphate (e.g., phospholipids) that may react irreversibly with the restorative surface and compromise bonding. This also contraindicates the use of phosphoric acid on zirconia restorations. To clean zirconia restorative surfaces after try-in and create an optimum surface for adhesive bonding compared to other cleaning protocols, a unique product (Ivoclean®, Ivoclar Vivadent, Inc.) is indicated.9,10 (See Figures 7 and 8.)


- The use of primers containing phosphate end groups or cements containing MDP (10-methacryloyloxydecyl dihydrogen phosphate) is recommended for achieving the best bonds to the zirconia structure. The self-adhesive resin cements (e.g., SpeedCEM® Plus) contain MDP, so the application of restorative primer as a separate step can be eliminated.
Finally, cement is extruded in the restoration, seated per path of insertion, and followed by polymerization of the cement according to the manufacturer’s recommendation. The translucency of the zirconia restorations depends on the material’s composition and thickness, and hence light attenuation through the restoration varies. Therefore, it is critical to consider these factors while selecting the cement options.
For opaque restorations, self-cure and dual cure cements are recommended, and it is extremely important to let the cement set on a self-cure mode before checking occlusion or making occlusal adjustments.
Results
Interest has grown in using zirconia for fabricating monolithic, full-contour restorations, particularly as different generations demonstrate new levels of optical and mechanical properties to meet dentists’ demands. The composition, mechanical properties, optical characteristics, and processing of these new zirconias are different from previous generations of the high-strength material, and are differentiated by a number of factors.
Today’s new zirconia materials enable dentists and laboratories to choose among options that can be milled to full contour, demonstrate acceptable aesthetics and translucency, and are suitable for clinical situations in which high mechanical stability, thin restoration walls, and natural aesthetics are essential. n
References
- Volpato Maziero CA, D’Altoe Garbelotto LG, Celso Fredel M, and Bondioli F. “Application of zirconia in dentistry: biological, mechanical and optical considerations.” Advances in Ceramics—Electric and Magnetic Ceramics, Bioceramics, Ceramics and Environment. 2011:397–421.
- Chen YW, Moussi J, Drury JL, and Wataha JC. “Zirconia in biomedical applications.” Expert Rev Med Devices. 2016 Oct;13(10):945–63.
- Nielsen RH, and Wilfing G. Ullmann. “Zirconium and zirconium compounds.” Ullmann’s Encyclopedia of Industrial Chemistry. 2010.
- Miyazaki T, Nakamura T, Matsumura H, Ban S, and Kobayashi T. “Current status of zirconia restoration.” J Prosthodont Res. 2013 Oct;57(4):236–61.
- Ramos CM, Cesar PF, and Bonafante EA, et al. “Fractographic principles applied to Y-TZP mechanical behavior analysis.” J Mech Behav Biomed Mater. 2016 Apr;57:215–23.
- Munoz EM, Longhini D, Antonio SG, and Adabo GL. “The effects of mechanical and hydrothermal aging on microstructure and biaxial flexural strength of an anterior and a posterior monolithic zirconia.” J Dent. 2017 Aug;63:94–102.
- Zhang F, Inokoshi M, and Batuk M, et al. “Strength, toughness and aging stability of highly-translucent Y-TZP ceramics for dental restorations.” Dent Mater. 2016 Dec; 32(12):e327–e337.
- Pinto PA, Colas G, Filleter T, and DeSouza GM. “Surface and mechanical characterization of dental yttria-stabilized tetragonal zirconia polycrystals (3Y-TZP) after different aging processes.” Microsc Microanal. 2016 Dec;22(6):1179–88.
- Kim DH, Son JS, Jeong SH, Kim YK, Kim KH, and Kwon TY. “Efficacy of various cleaning solutions on saliva-contaminated zirconia for improved resin bonding.” J Adv Prosthodont. 2015 Apr;7(2):85–92.
- Pathak K, Singhal S, Antonson SA, and Antonson DE. “Effect of cleaning protocols of saliva-contaminated zirconia-restorations: shear bond strength.” J Dent Res. 2015;94 (Spec Iss A):3656.