
PLANNING AHEAD MAKES LARGE CASE DENTISTRY PREDICTABLE.
“Simple extraction? There is no such thing as a simple extraction!” I once overheard an oral surgeon in dental school utter those words to an unsuspecting dental student who had made that erroneous claim. Like that student, dentists often put procedures into categories and subsequently choose the ones they are comfortable with to perform. In other words, “difficult” cases get referred out. While this may be the model that many dentists were taught in dental school, I was blessed by mentors who taught me to embrace the challenges of complete dentistry. This fundamental difference has made a tremendous impact on my practice. A periodontist friend of mine labels general dentists who practice comprehensive dentistry as, “restorative specialists.” This type of dentistry starts with one simple word—systems.
With appropriate systems in place, you have an entire world of dentistry to discover, enjoy and prosper from, while patients benefit from great care by a trusted dentist. Systems make procedures more predictable, less stressful and generally less time-consuming than procedures without such systems in place. Systems help build confidence in the skills dentists have and help your team have confidence in your leadership. Your staff will know you care about what you’re doing and the patient will also sense the pride you take in your dentistry.
One procedure that demands a system (and that most dentists refer out) is full mouth reconstructions. The numbers don’t lie. The vast majority of dentists have never completed a full mouth reconstruction. It sounds intimidating—daunting even. Thankfully, other dentists have already established systems that are . . . dare I say it . . . simple. Even full mouth reconstructions can be managed and tackled in an organized fashion.
One of the courses that helped me organize my approach and simplify the process was the Full Arch Reconstruction Course offered by the Dr. Dick Barnes Group. In this course, Dr. Jim Downs simplified the full mouth reconstruction process from treatment planning to finishing and photographs. Every case is different, but there are phases to each case that bring the doctor confidence and predictability. As I performed more full mouth and full arch cases, my systematic approach enabled me to visualize the entire case from start to finish and made it possible for me to enjoy the process rather than be intimidated by it.
Systems Case Study: Patient Mark
About four years ago, I met a patient named Mark. Mark was a hardworking gentleman who had a very difficult dental history and an equally difficult reconstruction to perform. Mark said that it took all his courage to walk through the door for his first appointment.
Mark came to my office in 2010 with pain on the lower left and it was determined that he needed a root canal, buildup and crown on number 20. We performed the procedure using IV sedation due to his extreme dental anxiety. Mark then had a complete exam, photos, FMX, and impressions and it was determined that he would be a candidate for a full mouth reconstruction. The important thing to note is that because I had already developed a systematic approach, I was able to see past Mark’s chief complaint, understand the comprehensive needs and provide a solution for his whole mouth.
Mark had been dealing with his dental problems using a piecemeal approach and was not receiving regular preventative care. One of the significant factors in this case was Mark’s heavy wear due to bruxism and the resulting collapsed bite. Mark was always uncomfortable and his masticatory muscles were 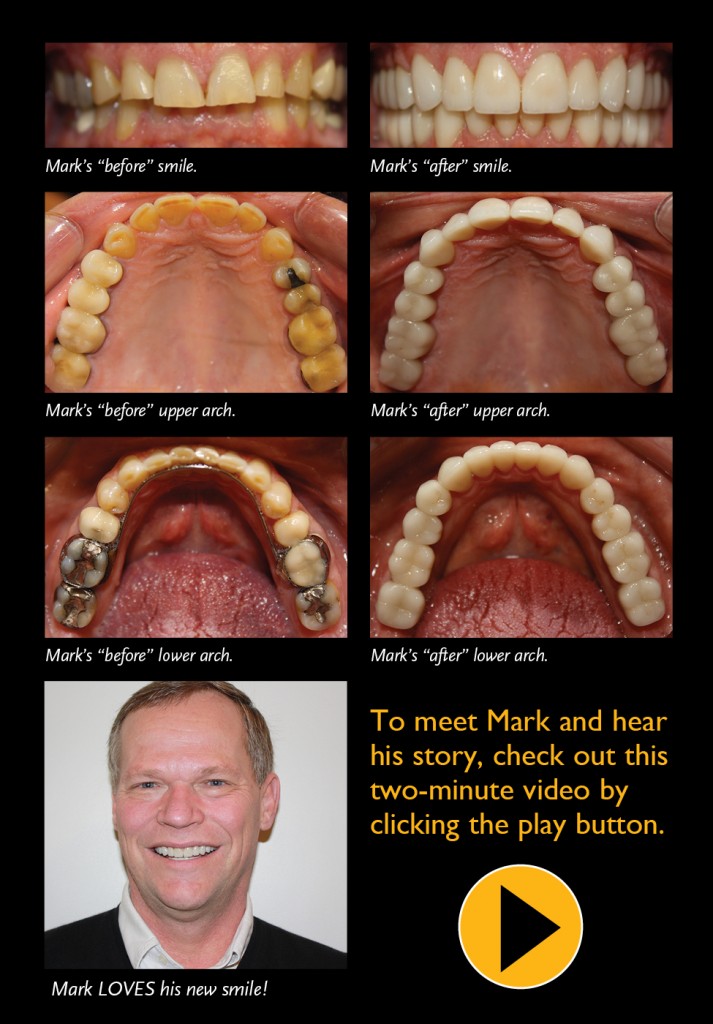 extremely tender and caused him continual discomfort. Headaches were the norm and required him to take daily medications. In addition, Mark had a significant infection on number 14, number 29 and number 30. Although Mark understood my recommendations, he was nervous to proceed and finances were a concern.
extremely tender and caused him continual discomfort. Headaches were the norm and required him to take daily medications. In addition, Mark had a significant infection on number 14, number 29 and number 30. Although Mark understood my recommendations, he was nervous to proceed and finances were a concern.
With Mark, if I had merely looked at his chief complaints, he wouldn’t have necessarily needed a full reconstruction. But when I systematically looked at his bite, looked at the wear and condition of the gums and the bone around the roots, this case was ‘screaming’ for a full mouth reconstruction. One of the key benefits of a systematic approach is that it causes dentists to slow down, go through the process and provide a comprehensive evaluation. The natural tendency is the opposite and focuses solely on the obvious problem.
Nonetheless, after his first visit, Mark disappeared, despite our follow-up calls. We simply told Mark, “When you’re ready, we’re ready.” As part of my approach, I do not pressure patients for treatment, which is very important. Yet, I always make sure—as Dr. Dick Barnes says—“to figure out the patients’ motivations.”
Two years later, Mark returned to the office. By then, number 30 was so painful that he was ready for treatment. In our consultation, we talked about Mark’s heart (he recently had a fifth heart stent placed), the infections in his mouth and how that can negatively impact other systems in the body. We talked about Mark being in pain every day. We talked about the desire to smile with confidence and look better. Every patient has internal motivations for moving forward and if dentists are in tune to what those reasons are, we can speak in ways that will resonate with patients. By understanding some of the underlying motivations, I was able to support Mark’s decision to move forward.
Shortly after that visit, Mark returned to my office with another toothache—that was the “last straw.” His finances were apparently in order and during the visit, his fiancé came with him for the consultation and encouraged him to move forward. “It’s time,” were the only words Mark needed from me.
As Mark’s case showed, a systematic approach was important because it enables dentists to see and identify all the areas of concern and present them in a comprehensive fashion. With an established system, dentists don’t have to convince the patient they need care. Establishing a thorough plan and an order in which to perform each step gives confidence to patients that they have selected the right dentist!
After Mark returned, the easy route would have been to simply say, “What would you like me to do for you?” Instead, we went through a defined process to create a vision for Mark for great dental health and great aesthetic results. We began with the necessary diagnostic records immediately. To complete the full mouth reconstruction, Mark’s appointments included almost every level of dental reconstruction.
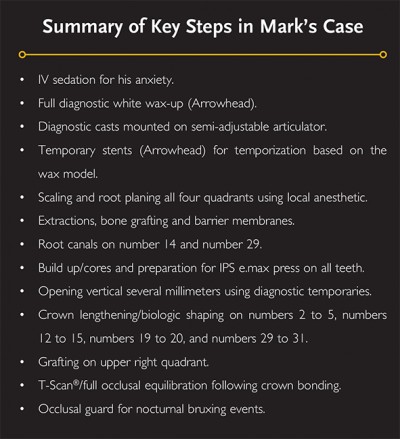 Here is a summary of some of the key elements in my process. Parts of the system merit a more in-depth analysis. I’ve included detailed explanations on selected parts of the system in the paragraphs that follow.
Here is a summary of some of the key elements in my process. Parts of the system merit a more in-depth analysis. I’ve included detailed explanations on selected parts of the system in the paragraphs that follow.
IV Sedation
When performing larger cases, patient comfort is a key component of my system. Starting with the first phone call, my staff is trained to evaluate the patient in terms of his or her need for sedation. Sedation isn’t just for patients with dental anxiety, it’s also utilized in my practice for cases involving surgery, long reconstruction appointments, sensitive gag reflexes and patients with TMD. Using sedation selectively allows me to be more productive in a single appointment, which benefits both the patient and the practice.
When Mark came into the office, he was so nervous, he could barely get through the door. Because the patient’s comfort is part of my systematic approach, I knew from the outset that we needed to use IV sedation for Mark’s extreme anxiety.
Full Diagnostic Wax-Up
The diagnostic wax-up is critical to identifying occlusal challenges and esthetic concerns prior to proceeding with treatment. It’s almost like having the patient in the office when they’re not! It’s great to have X-rays, but they are two-dimensional images of a three-dimensional object. Models are a great way to bring about a total understanding of the relationship of the upper and lower teeth and the condition of the teeth. Having a complete white wax–up of the case is also a powerful communications tool. It keeps the patient, myself and the lab focused on the desired outcome. When Mark saw his white wax-up for the first time, he was able to see a physical representation of the vision we had previously established. I use white wax-ups on all of my large cases—it is a key part of creating predictability in these cases.
Diagnostic Casts Mounted on a Semi-Adjustable Articulator
In Mark’s case, we were changing the occlusal landscape and increasing his vertical several millimeters. His attrition was significant and I wanted to know ahead of time if opening his bite would pose any challenges or create problems. Part of my system is starting with the end in mind.
Temporary Stents
When I have the white wax-ups fabricated, I also get a stent and a prep guide from Arrowhead. The stent makes the process of maintaining the bite simple and accurate. My dental assistants also use the stents to quickly make beautiful temporaries that mimic the wax-up model. At this stage, the patients are usually very excited because they begin to see what the end result will be. How many dentists would comfortably assign a fully prepped arch to their assistant to temporize? Many of my colleagues answered that they personally do this step themselves. With the white wax-up stent, it can be delegated with confidence!
Occasionally, I will use Arrowhead to fabricate another type of stent. It is a temporary occlusal stent designed to be worn by the patient during the temporary phase to help them adjust to their new vertical and to protect their temporaries from damage. Given his propensity for bruxing, Mark’s case included temporary stents.
Temporary stents are especially useful if you are doing single arch dentistry and a patient will not be finishing the opposing arch for a while. During the intervening time, a patient simply wears a stent to help mitigate any bruxing that could otherwise complicate a case.
Scaling and Root Planing
One of my system’s core beliefs is that the teeth we restore are only as good as the foundation supporting them. With Mark, the X-rays and probing depths at the very earliest appointments showed a significant amount of bone loss around different teeth on all four quadrants and some periodontal disease. So scaling and root planing go back to the foundation that I discussed earlier. Scaling and root planing not only remove plaque and calculus, which contribute to dental disease, they also smooth root surfaces, rendering them glassy and less likely for food and plaque to attach.
Bone Grafting and Barrier Membranes
Bone grafting is a way of both preventing bone loss and creating support areas for implants and soft tissue. Mark had areas that needed grafting. I wanted a strong platform of bone and soft tissue that was well adapted to the teeth and bone. The barrier membranes simply help hold the bone grafting products in place and keep the soft tissue from invading the surgical site while a patient heals following surgery.
Opening Vertical Using Diagnostic Temporaries
Opening Mark’s vertical helped with the attrition loss and in reconstructing the youthful look of his teeth. This approach also helps with muscle function, as muscles tend to be in a more chronically strained position when the bite has collapsed from wear over time. We were able to help Mark achieve a more stable bite and more attractive smile by adding vertical dimension to his case. Shimbashi studies confirm the benefit of improving vertical dimension and I always establish the VDO (Vertical Dimension of Occlusion) prior to prepping teeth.
Biologic Shaping
Perhaps one of the least emphasized areas of comprehensive dentistry and full mouth reconstructions is biologic shaping. While many dentists define this simply as crown lengthening, that isn’t accurate. The purpose of crown lengthening is to remove bone and lower soft tissue around a tooth in an attempt to “lengthen” the tooth. Biologic shaping involves the removal of old dentistry (including old crown margins), furcation issues, root irregularities and bony irregularities to create proper parabolic architecture of the bone and soft tissue around the tooth being restored. This means that often very little bone is removed at all!
Biologic shaping is a great way to create an ideal support structure around the teeth while simultaneously eliminating subgingival dentistry and making restorations easier to keep clean. We took this approach with Mark and as you can see, the results are just what we intended: healthy bone, healthy gums, healthy teeth!
Gingival Grafting
Another very important and often overlooked phase of full mouth reconstructions is the area of proper connective tissue around the teeth. Without connective tissue, teeth are highly susceptible to gingival breakdown and periodontal disease. Part of my system involves analyzing the health of the soft tissue around the teeth and identifying those areas that need connective tissue. Mark received grafting on the upper right quadrant. Failing to do this in Mark’s case would have increased the likelihood of future problems. Because we systematically addressed this concern as part of our process, it was easy to see exactly where this needed to be done for Mark.
Occlusal Equilibration with T-Scan® and Bruxism Guards
In my system, I include some additional steps that go beyond placement of the restorations. This is the ‘final piece to the puzzle,’ and sadly, one phase that many dentists skip. It consists of two key elements: occlusal equilibration using T-Scan® and the fabrication of a bruxism guard. Those two steps are my insurance policy that ensures the dentistry will last.
Once the final restorations are bonded in place, I begin the equilibration process using the T-Scan®. It takes the guesswork out of getting that new bite just right! Then we fabricate an occlusal guard to help the patient protect their investment against nocturnal bruxing events.
Mark was a significant bruxer so this was a must in his case. For him, the result was a beautiful smile that looks as good today as the day it was seated. The last two steps saved me countless hours in chair time that I would otherwise have spent fixing fractured crowns due to occlusion problems.
Overall Results
Since we completed his case last year, Mark is healthier, happier, and much more confident in his demeanor. He now says he loves to smile! What is that worth? For Mark, it is priceless.
For me, having a systematic approach for evaluating and completing full arch reconstructions has taken my practice to a whole new level. I don’t shy away from large cases and every complete reconstruction that I perform helps me gain more experience. I call each of these cases growing events. They are not always easy, but the challenges of such cases come with opportunities to grow in knowledge and skill; each one helps me refine my system so that the next case is that much easier. As a bonus, my confidence in single tooth dentistry has increased, too. Now, working on a single tooth area seems almost like a walk in the park!
This approach has also had a huge financial impact on my practice. Larger case dentistry has allowed me to attain higher levels of production and the referrals that these patients generate are a continual source of revenue. In other words, it is a win-win.
I encourage anyone who hasn’t completed a full arch or full reconstruction case to make 2014 the year you begin! Start by creating a system for full mouth reconstruction that is repeatable and focuses on helping you attain more predictable outcomes. If you don’t know where to start, I recommend attending the Full Arch Reconstruction Course taught by Dr. Jim Downs. Attending the Arrowhead courses will help you develop a system and make you a better clinical dentist.









