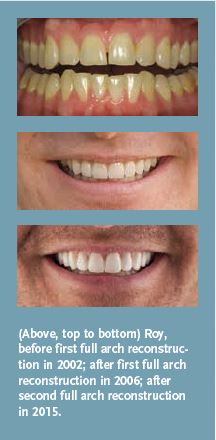
A Second Full Arch Reconstruction with the Latest Technology.
The expression “the third time is the charm” isn’t always true. Sometimes, you only need one or two attempts to succeed. I’ve had not one but two full arch reconstructions. While the first reconstruction wasn’t a failure by any means, the second full arch reconstruction truly gave me the smile I’ve always wanted.
Unlike many patients who want a full arch or full mouth reconstruction, I didn’t experience any major health problems or unbearably painful complications because of my teeth. I wasn’t teased about my smile as a kid, I didn’t suffer from headaches or other pains, and I wasn’t looking to repair damaged dental work. I was motivated to undergo a full arch reconstruction because I was just dissatisfied with the overall appearance of my teeth.
I also have a unique perspective because my job is working on other people’s teeth. Since 1995, I’ve worked for Arrowhead Dental Lab in Sandy, Utah. I started work as a dental technician (in the model and die department), and for more than 20 years, I’ve worked in just about every department at Arrowhead. For the past nine years, I’ve managed the ceramic department. In my current job, I oversee training for more than 60 ceramists and teach them how to create the best quality restorations.
Although I originally had my teeth reconstructed in 2002, the materials and techniques have advanced since that time. Therefore, I was anxious to upgrade to the latest materials and techniques that dentistry could offer.
New and Improved
When I first had my teeth done, Dr. Jim Downs from Denver, CO, was planning on teaching a full arch reconstruction course with the Dr. Dick Barnes Group and he needed a patient. Because I had some discolored teeth (they were yellower than I wanted), I volunteered. I became the patient for the course so I could get some veneers over my upper teeth and make them whiter. Then last year, 13 years later, Dr. Downs worked on my teeth again. I had a second full arch reconstruction because the materials had improved significantly and I wanted a new upgrade for my smile.
Originally, I had my teeth done with Finesse® restorations, which were made from all-ceramic porcelain. It is an aesthetically pleasing, but somewhat weaker, material with a higher fracture rate than more recently developed materials. When Ivoclar Vivadent launched the IPS e.max® system, which is stronger in the mouth, I wanted to change my restorations. IPS e.max® offers a more aesthetic porcelain combined with a stronger material that typically lasts longer.
Because I am a bruxer and grind my teeth, I had some fractures with the original Finesse® restorations. Once one broke, the others started breaking—so I decided to remake them all. The Finesse® restorations wouldn’t hold up to my bite, so I really needed something stronger.
During the most recent full arch reconstruction, I had the Finesse® restorations removed and I redid everything out of the stronger IPS e.max®. My entire upper arch was reconstructed again with the new materials. Dr. Downs put Snowcaps (see article, “Expedition Snowcaps: Discover the Multi-Purpose Case Solution,” Aesthetic Dentistry, Fall 2015) on my posterior lowers, and we plan to finish the lowers in the near future.
For my second full arch reconstruction, I was the seat patient during a full arch reconstruction seminar for the Dr. Dick Barnes Group in Denver, CO. I flew to Denver and Dr. Downs took off the Finesse® restorations, and then I flew back to Utah where he seated the restorations later during a bonding course.
As a dental technician, I am acutely aware of the teeth in my mouth. Most patients aren’t so attuned to every little nuance, but I notice every little defect. As a technician, it’s hard to imagine how small changes to the tooth will impact the feel in the mouth. But as the patient, I could see and feel every minor defect—things I didn’t realize were there until they were put in my mouth.
With a second chance, I was able to fix some of the original flaws. In addition, with the knowledge that I had gained throughout the years, I had a lot more experience and skill with the second set of crowns, so they were not only more functional, but they were also better looking.
After my first full mouth reconstruction, I noticed quite a few things that I wanted to change in the original crowns. For the second set, I wanted to dial in the occlusion and function even more, and I wanted to put different translucencies and effects into the crowns that were improved from the previous ones.
Additionally, after noticing the fractures on the original restorations (which I had to fix repeatedly), I really wanted something stronger. Because of my work with IPS e.max®, I had noticed how pretty and strong it is, and I really wanted to switch to e.max®. The fracture rate on e.max® is much lower than with Finesse®. The strength comes from a material called lithium disilicate, which is a well known type of glass ceramic. The strength of lithium disilicate (measured in megapascals, MPa) is far superior to many other restorations.
According to a March 2009 article in Dentistry Today, “The strength of ceramic material is about 80 to 100 MPa for metal ceramics, approximately 100 MPa for veneered zirconia, and 150 to 160 MPa for lucite glass ceramics. However, for the pressed lithium disilicate, the strength is in the range of 360 to 400 MPa.”
I made my own teeth for the restorations, so I know they will last. I didn’t put a lot of porcelain in the occlusion. I kept it all ingot, which makes it much stronger. Every time you add porcelain, the reconstruction is only as strong as that porcelain. Aesthetically, using ingot instead of porcelain is a bit of a compromise, but just a bit. It still looks good. The porcelain adds depth and translucency, but most people don’t see the occlusion. I wasn’t too worried because most of the “pretty” stuff is on the front where people see it.
I’ve been living with the new reconstruction for a few months now and haven’t had any problems at all—they seem to be holding up well. I haven’t noticed any problems or any issues. The difference in my smile is subtle enough that others don’t really notice it—the change was mostly for my own personal benefit.
Changing reconstructions from one material to another doesn’t account for a dramatic difference, as far as appearance is concerned. There are some translucency differences, but the differences are noticeable more often in the small details—the things you can’t see, but you can feel. I know that the teeth in my mouth are better than the ones I had before.
Just Doing My Job
I now have firsthand experience with what patients go through during large-case dentistry, and this experience helps me in my work. That’s why some doctors decide to get their own teeth done—so they can experience what their patients feel. Hopefully that level of understanding will lead to better diagnoses and doctors can better understand their patients’ needs and wants. It’s hard to completely understand what patients go through without having a reconstruction done.
The most surprising thing to me about the process (after the first reconstruction) was my occlusion. My first crowns had a nice, bumpy anatomy and looked natural. But in the mouth, natural teeth are actually slightly worn. Teeth don’t have that “virgin” anatomy—they are worn down every single day from use. As a result, the manufactured teeth felt unnaturally bumpy and sharp, and I always felt like I had “stuff” in my teeth.
For the second set of crowns, I made the teeth much smoother. They still have a nice, detailed anatomy, but they’re more smooth and functional. As a technician, learning to contour comes with experience, and learning such things as the Curve of Spee and the Curve of Wilson are critical to job performance.
As technicians, we’re taught (at least in our lab) to stack the anatomy in (which means to include the bumps and crevices similar to what is found on natural teeth). All the bumps and anatomy that techs include look pretty, but when they put it in the teeth, sometimes it doesn’t feel as pretty as it looks. If something is a bit off, it’s like having a sesame seed in your tooth—it may be small (almost imperceptible to the naked eye), but you can really feel it.
When we were stacking in the anatomy the second time around, I had learned about all of the things that felt uncomfortable or just a bit “off” in my mouth. Therefore, I learned what things can cause discomforts for patients and I learned to change up the techniques and adapt to this new knowledge.
Patient-Technician Advice
After undergoing a full arch reconstruction twice, the biggest thing I have learned is that for doctors and technicians to do their best job and be on the same page, there needs to be clear communication. Doctors should provide technicians with study models, shade tabs, and pictures. Technicians need those tools to make the tooth or teeth match the patient’s and doctor’s expectations.
Some doctors will send a shade and say, “A1,” and then it’s left to the technicians to guess the rest. At times, the majority of the technical work is guesswork. But for a doctor to be extraordinarily successful and to have fewer problems and frustrations, the technician needs to have study models, shade tabs, photos, the patient’s profile, and the patient’s expectations in advance. It’s extremely helpful for technicians to know what that patient’s expectations are for their restorations.
The better that doctors and labs communicate on such issues, the better the results will be for the patients—it makes it easier for doctors and the lab to deliver a slam-dunk case. Otherwise, doctors are just hoping for the best, and are letting someone else determine what the patient is going to look like.
My teeth perfectly matched my expectations because I worked on them! They were exactly what I wanted. The biggest difference from the original restorations (besides the material) is that I lengthened the teeth somewhat. They’re the same size and shape, so there wasn’t a lot to get used to. I didn’t make many changes to them, except for the incisor translucencies and effects.
My smile makeover gave me a greater understanding of what patients go through, and now I am able to perform my job better. I think every cosmetic dentist should consider having his or her teeth done at some point, because it opens up a whole new perspective. Doctors can’t completely understand their patients until they do it. But once they do, it’s a whole new world of understanding!









