
Multidisciplinary Dentistry for a Full Mouth Reconstruction.
I first met Jack at a football game at Butler Community College in El Dorado, Kansas. We were both watching the game and were chatting casually about football. Eventually the conversation turned away from the action on the field. Jack said, “I hear you’re a dentist.” He’d been to several dentists he wasn’t happy with, so I told him to come and see me. And even though Jack lived more than 150 miles away from my practice in Mission, KS, he scheduled an appointment and actually showed up for the exam.
During the initial exam, I was amazed at how little was left of Jack’s natural dentition. He was a strong bruxer and had ground his teeth down tremendously. I knew we needed to salvage what was left of his teeth before they got even worse—and we needed to do something as soon as possible. Initially, Jack was somewhat dismissive of my sense of urgency, but I kept reiterating that if he continued to lose teeth, he would need dentures.
In addition to losing his dentition, Jack was in constant pain. Furthermore, Jack said that he was so self-conscious about his teeth that he rarely smiled.
Coaching the Patient
Jack took a lot of convincing to address the problems in his mouth. He kept telling me just to “fix it.” I finally said that I couldn’t just “fix it” because it was like working on a flat tire. Jack’s problems couldn’t be resolved with superficial fixes. I explained that, like patching up a flat tire, making so-called “patches” over the problems in his mouth wouldn’t resolve the overall problem. Avoiding the major issues in his mouth wasn’t helping Jack live a healthy life, either.

![]()
To finally convince Jack to get the work done, I explained it to him in football jargon. I told him that we needed to do a Hail Mary pass or it would soon be too late. I told Jack that he needed a full mouth reconstruction with additional complicated dentistry.
In October 2016 I was planning on going to a Clinical Hands-On course for full arch dentistry with the Dr. Dick Barnes Group in Sandy, UT. Because it was a Hands-On course, I needed to bring a patient to the course. I asked Jack to be my patient and told him that we could address the problems of his smile with a comprehensive treatment plan. I said that it was a rare opportunity but that I knew this would really help him out.
Jack still seemed reluctant to commit to treatment. So I finally framed my argument around the health concerns. I told Jack that I honestly believed it was advantageous to his overall health and longevity. I reminded him of the old saying, “If I had known I was going to live this long, I would have taken better care of myself.” I explained that we needed to take care of his teeth so they would last for the rest of his life. I said that I’ve never heard a full mouth reconstruction patient say in hindsight, “I wish I hadn’t done it,” or, “I wish I had put this off a little longer.”
Jack has kids and is an active guy. I wanted him to be healthy and enjoy his life and his family for as long as possible. I also told Jack that improving his smile would likely help him out with his job. Jack works for Toshiba in medical sales. Having a new smile could transform his business.
Ultimately, I showed Jack what I saw when I looked in his mouth with the intraoral camera. And for Jack, seeing was believing. When Jack saw the myriad of problems that I saw, it started sinking in. He finally agreed to be my patient for a Clinical Hands-On course in full arch reconstruction in Denver, CO, with Dr. Jim Downs as the instructor.
Game Day Prep
I started preparation for Jack’s full mouth reconstruction last summer—in 2016. We got started as soon as possible because I knew I had to open his bite quite a bit. Jack had a Shimbashi (the vertical dimension of occlusion during closure) of around 12 mm, and eventually we opened it to about 17 mm.
We had to have a big opening if Jack could tolerate it. But honestly, I think he could have tolerated just about anything—I could have put a pair of shoes in his mouth and he would have said, “This feels great doc”—because he’s just one of those patients. But we had to put some protection on his teeth because he had such a strong bite, which is why he was wearing his teeth down.
Our first goal was to open the bite. So I took impressions, photos, and the bite relation and sent that information to Arrowhead Dental Laboratory.

![]()
To get Jack used to his new vertical, Arrowhead made him an orthotic that he wore all the time. While Jack was wearing it, I kept in frequent contact with him.
Soon after he started wearing the orthotic, Jack reported that he was sleeping better, his jaw felt great, and he was not having any discomfort. He wore the orthotic religiously. If Jack wasn’t eating, he was wearing it. Being such a compliant patient really helped out.
It took two or three weeks to open up Jack’s bite. Afterwards he mentioned that when he was chewing without the orthotic, it felt awkward to close his mouth. We had to retrain his mastication muscles to compensate for the new bite relation that we were trying to establish.
Arrowhead also made a White Wax-Up to give Jack a great visual of what was possible with his smile. Because Jack was somewhat reluctant to agree to treatment, the Wax-Up was great because it showed him the possibilities for his smile. It was uncanny how perfect it fit. My assistant, Kelly Strowig, and I worked hard to communicate as clearly as possible with Arrowhead’s lab and dial in everything for this case.
Arrowhead included a bite registration jig with the Wax-Up and all the things that helped the Wax-Up come to life.
The Big Game
Once Jack’s bite was opened up, we flew to Denver for the course. On the first day of the seminar, I prepped Jack for treatment. The prep work involved using a soft tissue laser to re-contour Jack’s smile and the gingival tissues.
We ended up increasing his vertical about six millimeters, and both Dr. Downs and I were amazed that it worked out so easily. We originally planned for four millimeters, but the extra two millimeters really made a huge difference in Jack’s new smile.
I was comfortable using the soft tissue laser to contour because I’ve been using a soft tissue laser for about 15 years. I do a lot of lasering for general contouring. Often, after a patient does orthodontics, his or her teeth look great, but minimal tooth structure shows because of the hyperplastic growth of some of the young tissue (due to the irritation caused by moving the teeth). With the laser I can redesign the smile line and the gumline to help make the smile “pop.”

I had to do quite a bit of gingival contouring on Jack. I was able to show the other participants at the course what I was doing. I knew we had plenty of gum tissue to work with, so we wouldn’t violate the biological width—because once you violate that, your patient will get inflammation no matter how beautiful the crown is.
The most unique part of the treatment was having to perform some endodontics on Jack. He had one tooth with a gold crown on it that we were planning to remove. I discovered it was from an endodontic treatment from many years ago, and they had casted the coat and the crown together.
I thought I was going to be able to take the crown off and build a new crown back up, but I couldn’t do that. I couldn’t even get the old crown off! I therefore decided not to damage the tooth any more by trying to get it off. Dr. Downs and I decided to prep it like it was a tooth, take a little bit more time with the prep, and then put a crown over the top of it. It took a little while to get there, but it worked out fantastic.
In 34 years of dentistry, I’ve never done anything like that. I prepped the gold crown by drilling down—and I got it to where I could get to some natural tooth margin.
As a doctor, you’ve got to be flexible when you get into unexpected situations. No matter how much prep you do, surprises usually happen. That’s why it’s important as a general dentist to be able to perform multiple disciplines of dentistry. After the gingival re-contouring, I prepared the rest of the teeth.
The next step was making temporaries for Jack. I treated each tooth so they weren’t sensitive, and then I placed a temporary crown mold on, trimmed up the temps, and adjusted the bite (although I didn’t have to do much adjusting).

![]()
In the End Zone
Arrowhead fabricated all the crowns while Jack was in temporaries. In November, Jack and I flew back to Denver to seat the permanent restorations. For Jack, I did half bonding and half cementation—some of the crowns in the posterior had to be cemented, and all the anterior restorations were bonded.
At the seating appointment, I took the temps off and tried on each of the crowns. I like to check them individually and then bond everything at once. For each individual restoration, I made sure all the margins were perfect, and when Jack closed his mouth the contour looked good. So everything was fantastic before the bonding and cementation began.
Next, I placed each crown. After placing all the crowns, I only had to adjust one little area between tooth number 6 and tooth number 7. That was it! And then I adjusted the margins and the contacts on either side, and those required only minor adjustments, too.
I cemented everything and cleaned him up, and then I reviewed everything and made a few tiny adjustments. I used the electronic bite registration program and could see where he was biting.
Today, Jack is still bruxing, so he wears a splint to protect his restorations. Jack is in Snowcap temporaries on his lower arch, and when I seat his lower arch, I plan to make him a more permanent orthotic.

![]()
Postgame Wrap-up
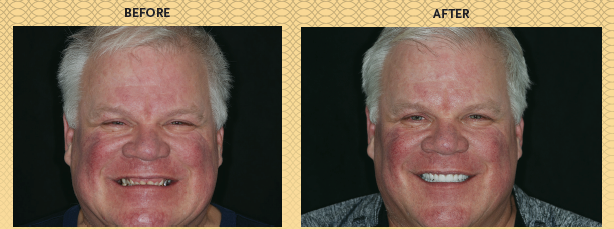
My favorite change is how often Jack smiles now. When he used to smile, it was almost like he was squinting. But by putting the facial muscles back to where they once were, Jack’s body immediately responded—he went from a tight smile to a relaxed one. Restoring Jack to his normal vertical bite was almost like giving him a facelift. It really made a difference in the way he looks.
When I spoke with Jack recently, he mentioned that people ask him all the time why he’s so happy! But it’s no secret. He knows it’s because of his new and improved smile. He remarked that he thinks his smile has helped to improve sales at his place of employment, too.
Because of the drastic changes we made to his bite, it took Jack at least a month to get completely comfortable with the new position of his bite. But now he says it’s fantastic.
Jack mentioned that he doesn’t even know how he could have functioned before. In addition, each of Jack’s kids have called me and thanked me for helping their dad. It truly shows how life-changing dentistry can be.









