
Using Monolithic Zirconia Restorations for a Full Mouth Reconstruction.
With greater public awareness about cosmetic dental reconstructions, dentists are often challenged with greater demands from patients. This increased demand for aesthetic restorative treatment challenges dentists, laboratory technicians, and dental manufacturers to develop techniques and materials to satisfy such discerning patients.
Utilizing digital planning, modern materials, and effective techniques, restorative teams can succeed in restoring a smile to proper form, function, and health. Recently, I completed a case that demonstrates the feasibility and significance of utilizing the latest techniques in planning, preparation, and material selection for a full mouth reconstruction of a patient’s dentition.
CASE PRESENTATION
An adult woman in her early 40s was referred to my practice by her dental provider because she was dissatisfied with the appearance of her smile. The patient commented that her existing teeth and restorations were unattractive because of recurrent decay, wear, and color (see Figure 1). Most notably, the patient mentioned that she was suffering from tension headaches, grinding, and a limited range of function.

At the first appointment, the initial diagnostic evaluation consisted of digital images with study casts, a centric relation bite record, a facebow transfer, and a full mouth set of X-rays.
In the maxillary arch, the patient had several teeth with worn composite and veneer restorations, as well as abfractions with cervical decay (see Figure 2).

![]()
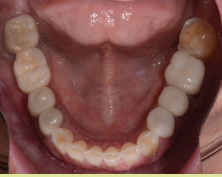
In the lower arch, several existing composite restorations had worn, and decay was exhibited on the facial cervical areas. Although there were no restorations present in the anterior mandibular teeth, there was severe wear in the incisal edges due to possible grinding and parafunction (see Figure 3).
![]()
PLANNING
After reviewing the clinical findings, as well as the mounted models, the patient was diagnosed with a restricted envelope of function and decreased vertical dimension from continuous and extensive wear.
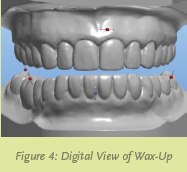
To develop a treatment plan and determine if the vertical dimension could be increased, a diagnostic 3D White Wax-Up (from Arrowhead Dental Laboratory) was fabricated. In the White Wax-Up, the patient’s vertical dimension was increased by 1.5mm.
Based on information gathered from the initial consult and digital images, we determined that the maxillary centrals could be lengthened by 1.3mm to improve the patient’s overall aesthetics. We determined that the canines would also be lengthened to restore canine guidance in lateral excursions. With regards to the patient’s lower anterior teeth, the goal was to correct the length-to- width ratio, and create a less-worn appearance.
As a result of the information gathered from the diagnostic Wax-Up (see Figure 4), I determine that aesthetics and function could be enhanced by restoring the patient’s entire dentition. The final treatment plan consisted of crown restorations, placing composite cores where needed from tooth numbers 2 to 15 in the upper arch, and tooth numbers 18 to 30 in the lower arch.
The material of choice for the crown restorations was Zenostar® (Wieland, Ivoclar Vivadent). According to the manufacturer, this translucent zirconia material combines excellent flexural strength with the aesthetics of natural tooth shades.
With full-contour Zenostar® restorations, there are two methods for achieving the desired shade: the Zenostar® brush infiltration technique, and the Zenostar® staining technique. Six pre-shaded zirconia blanks—pure, light, medium, intense, sun, and sun chroma—form the basis for reproducing the patient’s natural dentition.
Due to their warm, reddish nuance, Zenostar® Zr Translucent sun and sun chroma are suitable for restorations with individual color characterization, and can therefore be used for patients whose own natural dentition deviates from the classic tooth shades.
PREPARATION
After obtaining informed consent from the patient, treatment was initiated. First, we administered anesthetic to the patient and then removed any existing veneer and crown restorations. Then the teeth were cored with composite where there was any indication of recurrent decay remaining in the tooth. Adhese® Universal bonding agent (Ivoclar Vivadent) was applied following the manufacturer’s protocol, and cured using the Bluephase® (Ivoclar Vivadent) LED curing light.
Using MultiCore® Flow Light (Ivoclar Vivadent), build-ups were accomplished on the teeth requiring cores. A Clear Reduction Guide (by Arrowhead Dental Laboratory) provided with the 3D White Wax-Up was used to ensure adequate reduction for the definitive restorations. We used a coarse grit chamfer diamond bur (Komet®) to prepare the entire dentition for the Zenostar crowns starting from tooth numbers 2 to 15, and then on tooth numbers 18 to 30.
We took a full arch impression using Instant Custom C&B Trays (Good Fit®). Made of a proprietary material PMMA—poly(methyl methacrylate)—that becomes adjustable when heated in boiling water, these trays provided a quick, efficient way of capturing a dimensionally accurate impression with uniform thickness of the impression material. Once molded and customized to the patient’s maxilla and mandible, full arch impressions were taken using a heavy and light polyvinyl siloxane (PVS) impression material (Panasil®, Kettenbach).
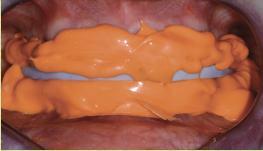
After the impressions were completed, a bite-relations jig was fabricated on the 3D White Wax-Up models (from Arrowhead Dental Lab) and tried in the patient’s mouth. Medium body impression material (Panasil®, Kettenbach) was placed into the relations jig and seated into the patient’s mouth on the prepared teeth (see Figure 5).
![]()
I asked the patient to bite into the relations jig until she reached the vertical stops and the material set. Instructions for the size, shape, and color of the final restorations were forwarded to the dental laboratory (Arrowhead Dental Lab), as well as the 3D White Wax-Up models.
Finally, a stump shade (Ivoclar Vivadent) was selected for shade-matching the preparations and to assist the laboratory technician in creating natural-looking restorations.
PROVISIONALIZATION
A provisional restoration, which aided in determining the best size, shape, color, and position for the definitive restorations, was made from a Sil-Tech (Ivoclar Vivadent) impression of the 3D White Wax-Up that was provided by the dental laboratory. Using a B1 shade of Visalys® (Kettenbach) temporary material, the Sil-Tech mold was quickly filled and placed on the patient’s prepared dentition (see Figure 6).

![]()
Within a few minutes, the provisionals were fabricated and effortlessly trimmed with trimming burs (Komet). Once the teeth were desensitized with Systemp® desensitizer (Ivoclar Vivadent) and then dried, the provisionals were temporarily cemented using Temp-Bond™ Clear (Kerr). The patient was given instructions regarding her home care routine with the provisional restorations, and regarding their use in eating, speaking, and biting.
A few weeks later, the patient returned for an evaluation of aesthetics, phonetics, and bite. She already exhibited excitement and confidence with her provisional restorations, commenting that all of her coworkers noticed that she looked younger and happier.
Most importantly, the patient said that she no longer experienced discomfort with her TMJ, and her bite had never felt better. Since no adjustment or modification of the temporaries were needed, the dental laboratory was instructed to replicate the 3D White Wax-Up when fabricating the definitive restorations.
LABORATORY CONSIDERATIONS
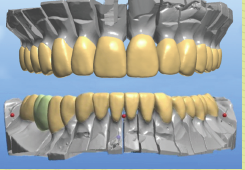
The 3D White Wax-Ups, color photographs, impressions,and bite relations were forwarded to Arrowhead Dental Lab. A scan of the 3D White Wax-Ups was used to selectan appropriate arch form, tooth size, and occlusion from the library of teeth available in the 3Shape Communicate™ software (see Figure 7).
![]()
Using 3Shape software, images of the proposed reconstruction were forwarded to my office via email. Any minor adjustments in tooth shape and contour were communicated to the laboratory’s technical advisor to achieve the ideal aesthetics. Once approved, the milling process began (see Figure 8).

![]()
CEMENTATION
Before try-in of the definitive restorations, the provisional restorations were removed using the Easy Pneumatic Crown and Bridge Remover (Dent Corp), and any remaining provisional cement was cleaned off the prepared teeth. The maxillary and mandibular zirconia restorations were tried to verify fit, form, and shade. After the patient was shown the retracted view for acceptance, we initiated the cementation process.
Riva Luting Plus (SDI), a resin-modified, self-curing, glass ionomer luting cement, was used for the cementation of the zirconia restorations, because it can be used without requiring special preparation (cleaning agents), nor does it require any bonding agents (see Figure 9).

According to the manufacturer, Riva Luting Plus utilizes proprietary ionglass™ filler. This material is a radiopaque, high-ion releasing, reactive glass used in SDI’s range of dental cements. Riva Luting Plus releases substantially higher levels of fluoride to assist with remineralization of the natural dentition.
This higher level of fluoride has a proven antimicrobial activity against three cariogenic bacteria: Streptococcus mutans, Streptococcus sobrinus, and Lactobacillus (1). In addition, Riva Luting Plus has low solubility in the oral environment, increasing the material’s ability to resist degradation and wear at the margins caused by oral acidity.
The preparations were washed and dried, so they were still slightly moist. Next, cement capsules were depressed consecutively to activate, and placed in the Ultramat 2 (SDI) amalgamator for only 10 seconds for trituration.
Using the applicator dispenser (SDI), the cement was loaded into the restorations starting from the midline and working distally. With a very low film thickness and a creamy consistency, the Riva Luting Plus cement was dispensed into the restorations with easy insertion and seating.
From this experience, Riva Luting Plus offers several advantages. With no etching, priming, bonding, or conditioning, it saves time. Because it’s hydrophilic, Riva Luting Plus works well in a moist environment. Additionally, the patient reported no postoperative sensitivity.
With Riva Luting Plus, it’s easy to remove excess cement, it releases fluoride, and it has low solubility in an oral environment. Excess cement was removed and cleaned up in about two minutes at the gel phase. After the cement was fully set (at five minutes), the occlusion was verified and adjusted.
The overall health and structure of the soft tissue and restorations was very good. The patient was extremely satisfied with the definitive results.
RESULTS
I checked the occlusion and verified it with the T-Scan® (Tekscan) to make sure that all the proper points of contact were in the ideal positions to ensure longevity of the reconstruction. The patient no longer experienced any pain and was very pleased with her new, enhanced smile (see Figures 10, 11, 12).

![]()

![]()

![]()
In addition, she commented on how effectively and efficiently our staff worked together in delivering her treatment.
Having a systematic method in place for treatment planning, material selection, tooth preparation, and cementation enables the dental provider to address the needs of the patient more effectively and efficiently. Because of this, the final outcome is much more predictable aesthetically and functionally.
References
Waldo B, Zhang P, Bennett J, Michalek SM, Katz J, Broome JC., Antimicrobial Activity of Composite-Resin and Glass-Ionomer Cements. University of Alabama at Birmingham, School of Dentistry, USA.









